An introduction to Digital Therapeutics (DTx) in global health and humanitarian settings
The Digital Therapeutics (DTx) for diabetes case aims to both deliver a patient support intervention and understanding of how DTx may supplement current MSF practices.Authors: Hanna Phelan, Ghinwa El Hayek
Person-centred care prioritises the preferences, lived-experiences and needs of patients and communities when designing and delivering health interventions. MSF is committed to becoming increasingly person-centred, working with people as partners and supporting more empowered health decision making. Digital health technologies known as digital therapeutics (DTx) are one way in which this ambition may be realised. Digital therapeutics are patient-facing platforms (typically a mobile app) offering evidence-based health behaviour change. By co-creating with patients and communities to leverage these DTx tools, patients will be able to more effectively access care and support, learn about their condition and treatment from a new perspective, and build improved practices to access improved quality of life and health outcomes. We are currently exploring and developing DTx for diabetes and DTx for tuberculosis (TB) in collaboration with multiple MSF associated clinics and communities to clarify the potential of DTx in contexts where the health burden is substantial and compounded by conflict, climate breakdown and other socio-economic factors.
This article introduces the foundational elements driving this work, defining DTx and its demand in relevant MSF settings, the case for person-centred digital health approaches, and a snapshot of the MSF DTx strategy.
Defining the DTx demand and value proposition
Before diving further into the detail of what a DTx tool is, it is important to pause on the challenges leading to its consideration at MSF. DTx was not assumed as a ‘solution’ for health challenges faced by MSF associated patients, communities and clinicians. We came to this point with a critical lens, looking closely at what is currently known about the technical, operational, cultural and social environments. Through needs assessments centred around interviews with patients and experts in addition to extensive desk research, long-standing barriers in accessing care and understanding were identified in two major areas of MSF’s work - diabetes and tuberculosis. It became clear that a DTx may be a promising tool to address a range of gaps including:
A demand for more integrated care approaches including an increased focus on mental well-being and behavioural elements,
A demand for increased ease of access at a distance for patients who were not able to regularly attend clinics or may have a need for added support between appointments,
A demand for increased focus on patient and community partnership,
A demand for timely and accurate data of vulnerable populations with these conditions where information gaps currently exist,
A demand for engaging patient education materials to aid improved condition and treatment understanding and more empowered decision-making,
In addition to what we were hearing and seeing in MSF projects in relation to diabetes and tuberculosis, and what is demonstrated in the literature, there is also a strong call for new ways of working at a global scale. Global health targets such as the Sustainable Development Goals (SDGs) underscore the scale of the issue. Goal 3 calls for coordinated efforts to “by 2030, reduce by 1/3 premature mortality from non-communicable disease (NCDs) through prevention and treatment and promote mental health and well-being.” The WHO have also recently announced the first global targets for diabetes coverage with a vision including that by 2030 80% of people living with diabetes are diagnosed, 80% have good control of glycemic, and 100% of people with type 1 diabetes have access to affordable insulin and blood glucose self-monitoring.
Similarly, the SDGs address the significant demand and ambition for TB systems improvements - “By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases” and the EndTB strategy calls for countries “to reduce TB incidence by 80%, TB deaths by 90%, and eliminate catastrophic costs for TB-affected households by 2030.” These global targets, driven by global needs, simply cannot be addressed without new and improved systems of patient care.
What is digital therapeutics (DTx)?
Digital therapeutics are patient support platforms used to encourage long-term behaviour change associated with chronic conditions such as mental health disorders, diabetes or hypertension. Oftentimes, and in the case of MSF DTx, bringing together a bundle of digital (patient-facing mobile platform and clinician dashboard) and in-person health management components including clinic appointments and community-based and peer support. However, some DTx tools may also exist as a standalone intervention not associated with formal clinical care.
In the MSF case, mobile-based DTx tools are provided as an adjunctive intervention to encourage improved patient understanding, and sustained behaviour change via multimedia education, goal setting, medication adherence and appointment reminders and remote monitoring of symptoms and side effects. Such tools differ from other patient-facing digital health applications (e.g., medication reminder apps) in terms of both the multimodal and holistic nature of features provided to the patient, commitment to evidence and impact and the integration within an existing clinical pathway.
Where needed and relevant, DTx can be used to enhance efforts for improved health, however, digital will not always be a fit. It is intended that the progress made with the MSF DTx project for diabetes and tuberculosis also contributes to operational improvements for those who may not want to, or cannot, use a DTx platform. This project intends to reduce the digital divide rather than add a new dimension to it.
MSF DTx approach
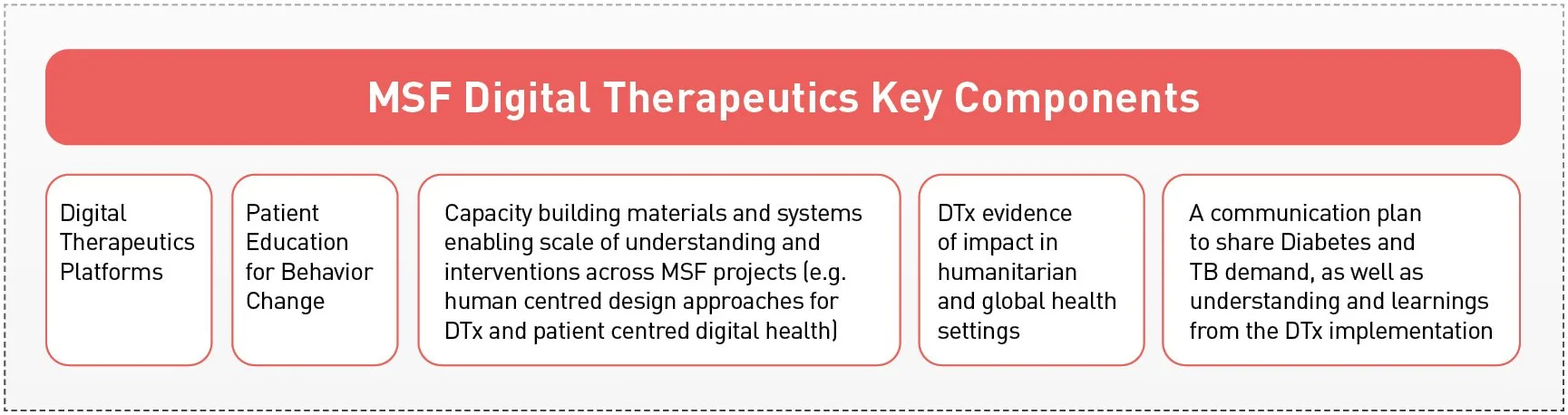
As alluded to the ultimate vision of the MSF DTx project is to improve access to high-quality person-centred care for patients living with diabetes and tuberculosis in low-resource and humanitarian settings. This will encourage an improvement in patient outcomes, quality of life and quality of care experienced. To do this we will continue to co-create and share tools, pathways and evidence with a multi-stakeholder group of patients, clinicians, Ministry of Health representatives, technical developers, and others to support patients to confidently self-manage their health between appointments.
A number of guiding principles for this work include:
● Patient centricity - inclusion of patients and caregivers throughout the programme planning, implementation, and evaluation with lived experience taken as priority
● Systems-focused - commitment to creating a tool that integrates with the current MSF system with minimal disruption to workflows and respects the complexities of the current ecosystem
● Privacy and Security - mitigation of risk and contribution to the development of new precedents for digital health privacy and security measures
● Accessibility - creation of interventions in both digital and non-digital formats where applicable to maximise access for patients and caregivers without technical means.
● Inclusion - Accessibility for those living with other impairments will also be considered and acted upon throughout the process (e.g. ensuring audio elements are available for those with visual impairments and/or low literacy rates)
● Evidence and impact generation - execution of the needs assessments, feasibility, and pilot studies to understand impact and disseminate learnings Advocacy and Communications - Contribution to evidence, learning and augmentation beyond the DTx element
This is a new endeavour for MSF with multiple projects under development and in-early implementation stages in multiple locations. While each step of this project demands forging new paths and processes it is clear that this effort is justified by the undeniable demand for MSF to scale up access to care that would not be possible through traditional practices.
The term ‘digital first’ has been increasingly used in recent years in conversations about the future of global and humanitarian health efforts. This term underscores the growing maturity of digital healthcare in acting as a new entry point for individuals and communities to access care. However from our perspective what is most promising is not a future of ‘digital first' but rather one of 'patient first’. This is the fuel of the current DTx projects at MSF.
This blog is the first series to be delivered over the coming year. The MSF SIU and collaborators will share unique insights into DTx with a focus on low-resource and humanitarian contexts. This exploration will include looking deeper into the health demands driving this work, reflections on the process and its theoretical underpinnings and evidence generated through operational research along the way. Stay tuned.