Prioritizing People with Lived Experience as Partners to Co-Create a Diabetes Digital Therapeutic (DTx) in Lebanon
Authors: Hanna Phelan, Ghinwa El Hayek, Dr Djoki Bahati, Tania Hachem, Cyrine Farhat, Josephine Mukamuganga, Dr Beverley Preater, Dr Sawsan Yaacoub, Maysaa Hellani, Sophie Wodon
Within a traditional biomedical model, focus is largely placed on the disease and associated treatment to reduce or alleviate symptoms experienced by a patient. This model falls short for people living with chronic conditions, such as Diabetes. Despite first being conceptualised in the 1970s, the biopsychosocial model, which emphasises the integration of the biological, psychological and social needs of people, has not yet been optimally embedded within global and humanitarian health activities due to several challenges associated with mounting complexity and lagging prioritisation.
For physical and mental health outcomes to improve via chronic condition-focused health programmes, there must be a shift away from seeing people as a set of symptoms, to thoughtful consideration of the whole person including their behaviours, beliefs, and realities. To succeed in delivering this integrated approach, the perspectives and preferences of people with lived experience are fundamental. In the setting of complex and compounded crises, the biopsychosocial model is particularly important to make necessary adjustments for effective service delivery.
Aligning with the evidence on the possibility to further improving quality of care and quality of life through integrated and person-centred initiatives, in addition to the rights-based and moral impetus, MSF strategic programming has increasingly prioritised patients and populations as partners. This approach engages with patients, their communities, caregivers, and MSF clinicians and staff, as partners in the design, implementation, and evaluation of healthcare services. Following the precedent of this strategy, the recently launched Diabetes DTx project, in two MSF clinics in Aarsal and Hermel, Lebanon, is intended to support People Living with Diabetes (PLWD) through integrated and participatory methodology, to confidently self-manage their condition between clinic visits.
This blog outlines the theoretical grounding associated with the DTx intervention co-creation with PLWD and clinicians and shares the knowns and unknowns of this project approach through quotes and insights from the different stakeholders involved [1].
Co-creation and participation in practice
Through meaningful health system engagement, individuals and populations are not treated as patients or ‘beneficiaries’ of aid but as active stakeholders and experts of their situation. Several concepts and resources have been developed to guide the operationalisation of this type of engagement, including the recently launched WHO framework for meaningful engagement of people living with noncommunicable diseases, and mental health and neurological conditions.
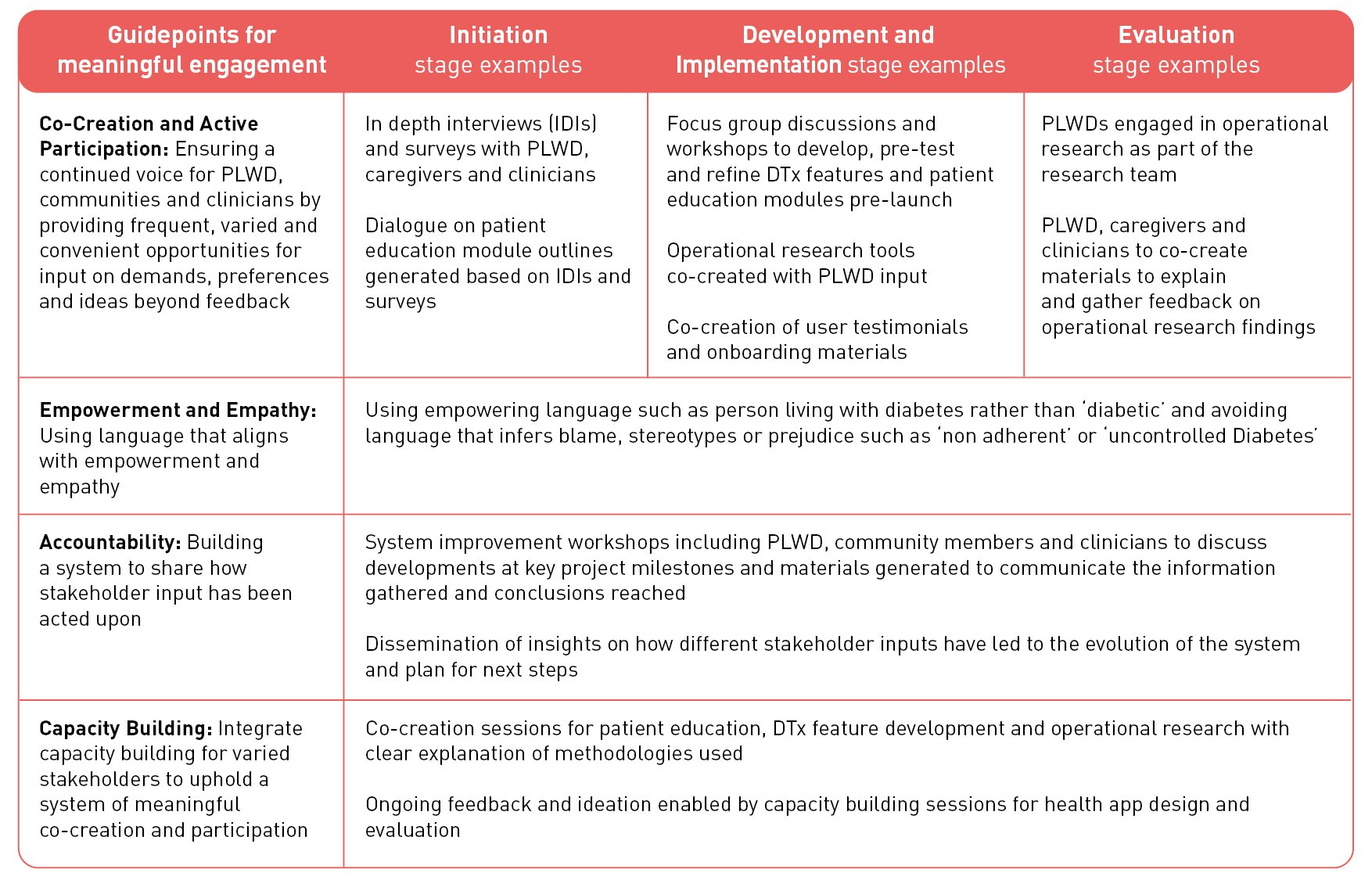
Although there is widespread consensus that engaging with PLWD and their communities is valuable in designing effective and sustained health services, there is a tendency to use terms such as ‘patient-centred’ in a somewhat tokenistic manner, approaching people with lived experience as a transactional exercise to claim a label, rather than a meaningful engagement built on mutual respect. Several concepts are being explored in the Diabetes DTx project to demystify meaningful engagement and translate the commitment of working with patients and populations as partners into action. A degree of this is briefly outlined in table 1 below.
The user-centred design component of this project, involving both PLWD and clinicians, is being built to ensure all elements of the intervention are sensitive to the specific context in which the intervention is intended to be deployed in Lebanon. Tania Hachem, the Medical Polyvalent Responsible calls this to attention saying:
“Clinicians and PLWD have first-hand experience with the challenges and needs of managing diabetes. By involving them in the design process, the DTx tool can be tailored to meet their specific needs and preferences, ensuring that it is user-friendly and effective.”
The project team includes Cyrine Farhat, a person living with Type 1 Diabetes in Lebanon and Founder of Positive on Glucose, who is reinforcing the voice of those with lived experience calling to attention the need for considered use of language in the content featured within the tool and guiding the design and testing of technical features.
“The language used in addressing people living with type one diabetes can have a significant impact on their emotional well-being and self-esteem. Using person-first language and avoiding stigmatizing or blaming language can help individuals feel empowered and motivated to manage their condition effectively.
Having a person with lived experience of type one diabetes on board can make a valuable contribution to shaping diabetes care by providing unique insights into the daily challenges and experiences of living with the condition. PLWDs perspective can help ensure that the project is more patient-centered, relevant, and effective in meeting the needs of those living with diabetes.”
The Diabetes DTx project is in the early stages of development and the practice of co-creation with end-users as a priority is still evolving, as a relatively new concept in the global health and humanitarian health space. The Information, Education, Communication, and Health Promotion Manager in Bekaa, Josephine Mukamuganga, acknowledges that moving towards the concept of having PLWD and their communities as partners is a learning process for both MSF projects and the Diabetes DTx project:
“In our project design [MSF projects], we are not yet at the patients as partners stage […]. People still ask us all the time why we did this and not that […]. We cannot change our programs overnight, but we need to listen more to and empower patients. They [patients] should know that being sick does not remove your value as a human”
The co-creation processes are not only about active participation of the stakeholders but also involves their capacity building, empowerment, contextualization, and accountability to populations as noted in Table 1 – this has the potential to not only influence individual projects but gradually shift the broader dynamic of healthcare engagement. Sophie Wodon, the PSEC and Health Advisor in the MSF Operational Centre in Geneva sees the value in taking time to invest in this process saying, “The patients and their families become actors and decision makers in their care”.
The benefit of working closely with patients and communities goes beyond the design of the technical features and therapeutic education content. It may also reinforce the ethical and privacy components which are key considerations for any technology or operational research engagement.
“People living with diabetes have a unique perspective on the ethical considerations surrounding the collection and use of personal health data. By involving them in the development process, the DTx tool can be designed with privacy and ethical considerations in mind, ensuring that it meets the expectations of both clinicians and patients.” Tania Hachem, the Medical Polyvalent Responsible
Overall, this methodology will look different at various points in the DTx project journey – at some stages co-creation may be sharing details on the challenges faced by end-users, at other points in the process it may be the creation of self-directed patient education materials or determining questions to be asked to the broader group to determine acceptability and usability of the tool (Table 1). So far, clinicians and staff working in the MSF clinics in Bekaa, recognize the value in the co-creation of this tool with PLWD in making the most of the limited time available to spend together during clinic visits.
“The DTx tool is intended to improve the way we [clinicians and MSF staff] spend time with patients, and take into account their considerations, and how we make patients actively participate in their treatment, as well as allow clinicians to interact with their valuable time” Josephine Mukamuganga, IECHP Manager-Bekaa
Clinicians are involved in the co-design process given their medical knowledge, familiarity with their patients, communities’ and the context they operate in to enable the resulting tool to extend the reach of the pre-existing trust and collaboration between the MSF team and PLWD “We can help to tackle how and what are the tools and information that are the best to address to patients, due to our observations in consultations, and familiarity with each patient. This relationship needs time to be built.” Dr Sawsan Yaacoub, Paediatrician working with DM1 patients.” As stated by Tania Hachem “Clinicians have the medical expertise needed to ensure that the DTx tool is safe, effective, and clinically appropriate.”
Involving the different stakeholders is indeed key for the uptake and subsequent adaptation of the project and to ensure a digital solution is appropriately embedded within the broader system to allow for sustained use, feedback, and buy-in “When people feel involved in the development process, they are more likely to feel invested in the product and use it consistently. By involving clinicians and people living with diabetes, the DTx tool can be designed to address their specific concerns and preferences, leading to better engagement and outcomes.” Tania, Medical Polyvalent Responsible
The inclusion of digital health tools and participatory approaches in the humanitarian and global health sectors is not new, however it must be acknowledged that there are nascent elements of bringing these items together, introducing some challenges. A major one apparent from the outset of the Diabetes DTx project is the length of time required to explore, define and implement these efforts. Ensuring all stakeholders see and understand the value of this investment of time is of high importance. The DTx project aims to empower both clinicians and PLWD through giving them a voice and a role for better quality of care and health outcomes and this inevitably takes time.
“The DTx is designing a modern application that facilitates a lot of the core patient education and support that we aspire to provide as doctors. Technology helps us to expand and extend our finite effective time with the patient, to continue the patient education, empowerment, gentle reminders for wholistic self-care beyond the office and into the community setting. It is a modern way to address the pandemic of diabetes particularly in humanitarian setting where in-person interface with a physician or health care provider is extremely limited." Dr Beverley Preater, NCD Doctor in Bekaa
There are certainly aspirations for this project to support PLWD to achieve improved mental and physical outcomes and to support clinicians to extend the reach of their care. As Lebanon grapples with multiple complex crises affecting all aspects of livelihoods for people living there, this intervention comes at an important time for PLWD who are struggling to access adequate care, guidance and medications. While the digital component is hoped to be relevant to as many people as possible it is inevitable that for others (for example those without phone access) this process ensures added value beyond the delivery of a digital solution alone. “PLWD will be more motivated and responsible, especially adolescents, as technology is central to them, all our [adolescent] patients are holding phones. They will be active and enthusiastic to have an alarm that can remind them of all details related to their condition. It will be a great chance for all PLWD [treated by MSF in this context] to have an improved self-management approach, which helps them increase their self-confidence, reflecting positively on their health because they will take care more of their body, signs & symptoms and their diet.” Maysaa Hellani, Clinical Nutritionist
Ending on the words of the Lebanon Medical Coordinator Dr Djoki Bahati ”For many years (still today), there has been a paternalistic dynamic within the medical field with health professionals telling people what to do or not to do and this is proven to be not efficient. Involving clinicians and people living with diabetes in Co-creating the DTx tool fosters people centeredness by incorporating elements seen from people's perspective. And this gives a chance to create an effective tool which responds to the real needs of people.”
[1] It is important to note that while the team has engaged with PLWD and their family members on many occasions for input, quotes from this group have not been included in this blog. With informed consent and necessary ethics approvals these insights are intended to be shared in subsequent external publications.