How digital health can accelerate access to diabetes education and care
Authors: Hanna Phelan, Ghinwa El Hayek
World Diabetes Day provides us with an opportunity to spotlight the substantial, and growing, global health demand for Type 1 and Type 2 diabetes care and a chance to share an insight into the MSF Sweden Innovation Unit’s (SIU) focus on supporting people living with diabetes in humanitarian settings using digital therapeutics (DTx). This year’s theme, ‘access to diabetes education’, is a part of the multi-year theme of 'access to care'. These themes underscore foundational fault-lines faced by people living with diabetes around the world - in particular those in low resource settings - and an indication of where those seeking to augment systems for true impact on patient experience and outcomes must maintain a determined focus.
Revisiting the diabetes demand
As with any dialogue on potential new solutions or processes, it is important to start with a focus on the demand. Diabetes is a major element of the global non-communicable disease (NCD) epidemic, with 6% of the world’s population estimated to be living with either type 1 or type 2 diabetes[1]. Low-and Middle-Income Countries (LMICs), where access to care is often a challenge, carry a large proportion of this global burden with 3 in 4 adults with diabetes residing in these contexts[2]. It is estimated that there are 4 million people living with diabetes displaced either as refugees or internally displaced (IDPs) as a result of man-made and natural disasters[3].
Organisations responding to humanitarian crises have unfortunately been slow to recognise the importance of including diabetes support and care within their emergency planning despite diabetes presenting a significant risk amplifier in scenarios of the climate crisis, political unrest and infectious disease outbreaks [4] . While the funding for NCD care is often insufficient in humanitarian settings a lack of proper epidemiological data on diabetes in their scenarios further impedes the decision-making for humanitarian actors in terms of interventions and raising funds[5-7].
In many settings where humanitarian crises occur, diabetes care is not widely available, due to, among other reasons, a lack of human resources for health, barriers to accessing clinics, and high cost and limited supply of medications and tools for diabetes care such as insulin and blood glucose monitors. For people living with type 1 diabetes, or those dependent on insulin, this lack of access can be a “death sentence”[8]. In the long term, for people living with type 2 diabetes, lack of access to care and sufficient education may lead to serious health complications such as kidney failure, heart disease, stroke and vision loss contributing to premature mortality and significantly reduced quality of life. Despite the discovery of insulin taking place over 100 years ago, it was estimated by the WHO that 50% of people living with type 2 diabetes still cannot access this lifesaving medication[9].
While access to medications, such as insulin is crucial for those living with diabetes, the outcomes and experiences of people living with diabetes are also determined by access to quality health education provided to enable patients and caregivers to support self-management and avoid diabetes-related distress and avoidable complications. Given the heterogeneity of patients and their circumstances and the complexity of diabetes treatment and management, generating and ensuring access to engaging patient education which empowers patients to be the experts in their own health must be prioritised.
Digital health for diabetes care access and education
Digital health approaches offer tools to increase the reach of health services and support and a new way to deliver community and patient education. However, to date, the scale of digital health implementations and quality of evidence generated has been limited in low-resource and humanitarian settings despite the aforementioned demand.
The digital health environment offers a plethora of tools and approaches relevant to diabetes including;
Telemedicine consultations for remote patient support and clinician supervision and training.
Medication adherence mobile applications for medication reminders and patient reporting.
Digitally supported community healthcare workers using mobile-based decision support systems.
Digital health promotion campaigns to encourage awareness of diabetes identification, management and destigmatisation.
Clinical decision support tools (eCDSS) to support diagnostics in remote settings without direct specialist care e.g. advanced imaging for diabetic retinopathy.
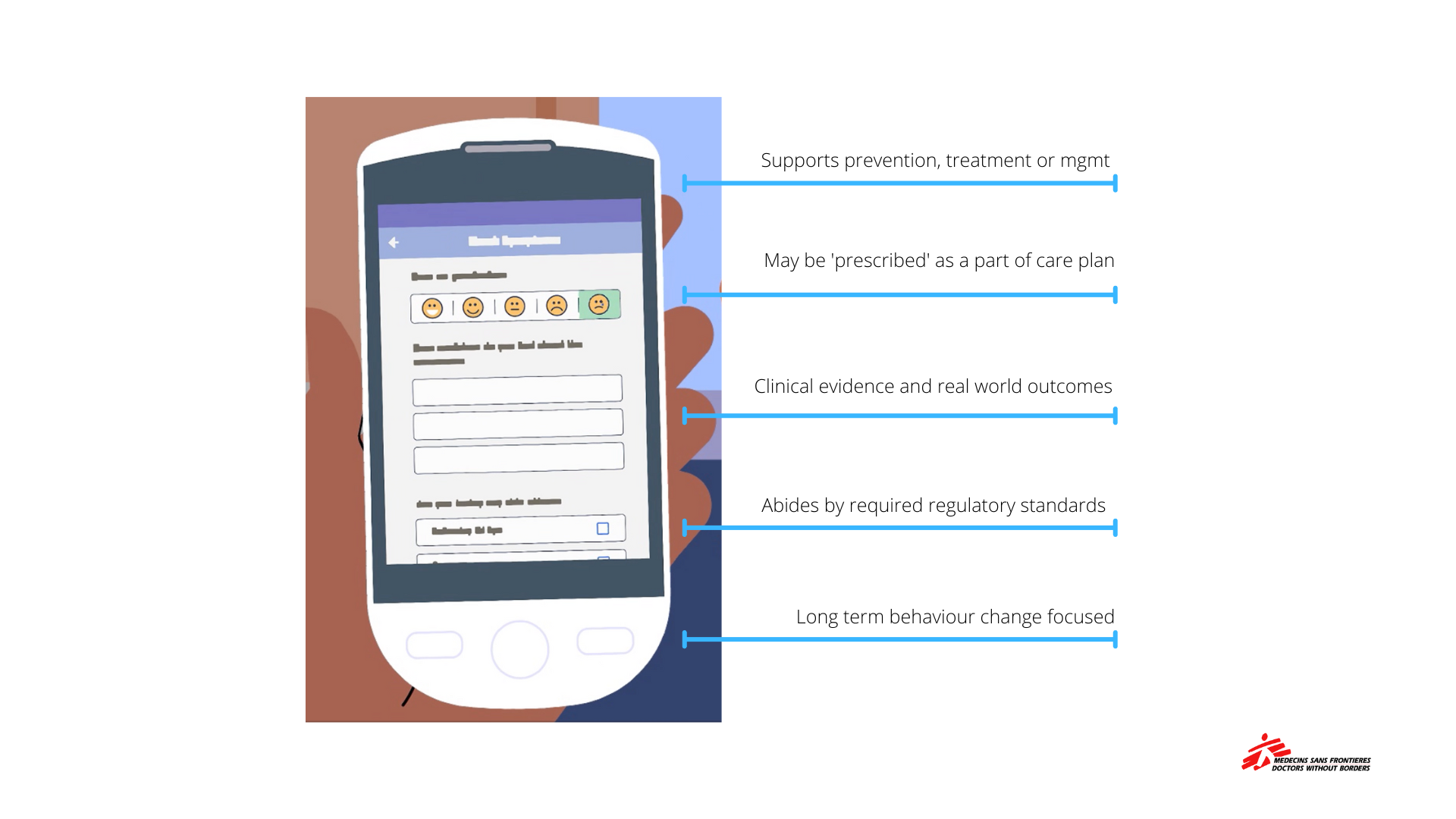
Digital therapeutics (DTx) Behavioural health tools, which may be integrated or ‘prescribed’ through conventional care pathways to support patients to more confidently self-management with the remote support of clinicians.
The MSF Sweden Innovation Unit is currently focused on the development and validation of a DTx for people living with Diabetes in the MENA region. Co-created alongside patients and colleagues in Lebanon and Geneva, this intervention will offer patients a companion tool for use between clinic visits to build understanding and increase connectivity with MSF services in the initial stages of diagnosis and treatment. Operational research will be conducted throughout this process to both provide evidence on the technical feasibility of the DTx for Diabetes in this context and also an insight into the impact of new forms of patient education delivered via the app.
While the primary focus of this short blog is to highlight some digital health interventions which may be leveraged to support expanded and quality access to treatment and support for people living with diabetes, it goes without saying that innovation does not necessarily have to be an entirely novel technical intervention. Innovation to support people living with diabetes may be a reimagining of an existing process, which may take various forms such as:
Integration of mental health services as a part of standard diabetes treatment,
Peer support with people living with diabetes networks to share learnings between those with lived experience,
Creative health promotion campaigns for the prevention of Type 2 diabetes through lifestyle modifications
Increasing access to previously developed and validated innovations (e.g. insulin and continuous glucose monitors)
Increasing access to quality diabetes care and education must be addressed with a creative systems approach. Through collaborative and evidence-based efforts a reality where no person with diabetes is left behind is possible.
The International Diabetes Federation launched in 2020 a multi-stakeholder initiative to encourage action, improve health services and ensure access to essential medicines for displaced people with diabetes. The objective of the call is to guarantee uninterrupted access to diabetes medication and care for all displaced people with diabetes and integrate diabetes care as a key component of the humanitarian response.
Source: International Diabetes Federation [1] World Health Organization. (2022). Noncommunicable Diseases Progress Monitor 2022. Retrieved from https://www.who.int/publications/i/item/9789240047761: [2] International Diabetes Federation. (2021b). Diabetes around the world in 2021. IDF Diabetes Atlas.[3] International Diabetes Foundation. (2020, June 30). Preventing and managing diabetes in humanitarian settings. International Diabetes Federation. Retrieved November 10, 2022, from https://idf.org/our-activities/humanitarian-action/diabetes-in-humanitarian-settings.html[4] Burki, T. (2022). Diabetes in humanitarian crises. The Lancet Diabetes & Endocrinology.[5] Roberts, B., Ekezie, W., Jobanputra, K., Smith, J., Ellithy, S., Cantor, D., ... & Patel, P. (2022). Analysis of health overseas development aid for internally displaced persons in low-and middle-income countries. Journal of migration and health, 5, 100090.[6] Ansbro, É., Issa, R., Willis, R., Blanchet, K., Perel, P., & Roberts, B. (2022). Chronic NCD care in crises: A qualitative study of global experts’ perspectives on models of care for hypertension and diabetes in humanitarian settings. Journal of migration and health, 5, 100094.[7] Kehlenbrink, S., Smith, J., Ansbro, É., Fuhr, D. C., Cheung, A., Ratnayake, R., ... & Roberts, B. (2019). The burden of diabetes and use of diabetes care in humanitarian crises in low-income and middle-income countries. The Lancet Diabetes & Endocrinology, 7(8), 638-647.[8] Burki, T. (2022). Diabetes in humanitarian crises. The Lancet Diabetes & Endocrinology.[9] https://www.who.int/news/item/12-11-2021-new-who-report-maps-barriers-to-insulin-availability-and-suggests-actions-to-promote-universal-access